AAMP
Chronic wasting disease: what hunters and processors need to know and do

Chronic Wasting Disease (CWD) is a contagious neurological disease that affects deer and other cervids. CWD is classified as a transmissible spongiform encephalopathy (TSE) disease also known as a prion disease. Prions are misfolded cellular proteins located on the surface of cells that infect and change other cellular proteins as they spread and accumulate in the body. It is not yet understood exactly how the prion proteins (PrP) are infected and structurally changed but once infected, CWD and all other TSEs are, after a prolonged incubation period, irreversibly fatal. As the prions accumulate in the brain, microscopic holes called vacuolar degenerations develop giving the brain a sponge-like appearance, hence the name "spongiform" (see Figure 1).

Figure 1: A comparison of healthy brain tissue (left) and tissue showing signs of vacuolar degenerations, astrocytosis, and amyloid plaque accumulation common to TSE diseases (right).
The structural changes that occur to the prions make it so that they cannot be destroyed by the body’s immune system, nor by other physical conditions, including protease (protein enzyme) digestion, cooking, cleaning or sanitizing processes. Scrapie, bovine spongiform encephalopathy (BSE) also known as “mad cow disease”, Creutz-feldt-Jakob Disease (CJD), and Kuru are other examples of TSEs.
Origins
CWD was first identified in 1967 in a closed herd of captive mule deer in northern Colorado. It became classified as a TSE in 1978 and later discovered in free-range cervid herds. Since then, CWD has spread all across the United States, Canada, and even beyond North America to Scandinavia and South Korea. There is still a considerable amount unknown about the disease like its origins, exactly how it develops and moves in the body (pathogenesis), how it persists in the environment, its ability to spread to non-cervids and how to inactivate the prions themselves.
Host Range
Cervid species found to be infected or susceptible include almost the entire Cervidae family:
- White-tailed deer
- Mule deer
- Eurasian red deer (experimentally)*
- Sika deer
- Fallow deer (experimentally)*
- Asian muntjac (experimentally)*
- Caribou
- Elk
- Moose
*Cells shown to be susceptible to infection through in vitro (outside the living organism) experiments. All other animals have shown infection in vivo (inside the living organism) in captivity or in the wild.
Pathogenesis in Natural Host
The pathogenesis of CWD is mostly based on knowledge and research from other TSE diseases. The progression of infection can vary depending on the species infected. After ingestion by the host organism, the prions progress through the gastrointestinal system to the lymphatic system and onto the central nervous system where they begin to accumulate. Once the prions reach the brain, they collect primarily at the base of the brain stem (the obex of the medulla oblongata). It is thought that the onset of CWD’s symptoms begin in conjunction with the prions reaching and accumulation within the brain and spinal cord. As time goes on, the infection will spread out from the central nervous system and begin accumulating throughout the rest of the body (Table 1).
| Tissues Confirmed Positive for CWD | Tissues Suspected or at Risk for CWD Infection |
| Brain | Mucosal Membranes |
| Pituitary Gland | Salivary Glands |
| Spinal Cord | Tongue |
| Eyes (optic nerve, ganglion cells, retina) | Intestines |
| Tonsils | Liver |
| Heart | Kidneys |
| Lymphatic Tissues (associated with the head, neck, joints, digestive system and rectum | Bladder |
| Spleen | Urethra |
| Pancreas | |
| Adrenal Glands | |
| Peripheral Nerves (near the spinal cord) |
Table 1: Cervid Tissue Proven or Suspected to Harbor CWD Prions
Pathological Signs
CWD is a slow-developing disease with a prolonged incubation time. The minimum incubation period of CWD (from exposure to onset of detectable clinical signs) appears to be 16–17 months, with periods up to 25 months observed in captive animals. Most animals are asymptomatic carriers meaning that the animals are infectious while showing no sign of the disease. Signs early on could be easily missed because they can be mistaken for normal behavior or seasonal body mass fluctuations. The clinical signs become more pronounced and noticeable towards the end of the disease’s course. (Figure 2).

Figure 2: A white-tailed deer displaying weight loss and roughened haircoat (left) and an elk displaying altered posture, droopy head and ears, and sialorrhea (right).
Another unique trait of all TSEs is that because the body’s immune system still recognizes the abnormal prions as apart of itself, no inflammatory response is mounted. The disease can effectively “hide” in plain sight in the host’s body. The earliest clinical signs include behavioral and subtle changes in movement:
- Impaired balance and coordination (Axatia)
- Altered posture (wide-based stance), and abnormal head carriage (droopy head and ears)
- Blank facial expression
- Head tremors
- Listlessness
- Behavioral changes
- wild cervids may lose their fear of humans and "tame" cervids may become aggressive
As time goes on, more specific and telling signs appear:
- Progressive weight loss
- Despite weight loss being a hallmark symptom of the neurological disease, it is often a late-stage sign. Many cervids may die with an average body weight and body mass before this clinical sign being expressed.
- Roughened haircoats (poor thrift) and/or retention of the winter hair coat
- Excessive teeth grinding and jaw clenching (bruxism)
- Excessive drooling and salivating (sialorrhea/ptyalism)
- Excessive eating and hunger (polyphagia)
- both despite the loss of weight and muscle mass
- Extreme thirst (paradoxical polydipsia)
- despite the animal staying hydrated
- Excessive urination (polyuria)
- in combination with paradoxical polydipsia contribute to late-stage shedding of infectious prions through urine
Since all signs of CWD can occur in conjunction with other diseases, it cannot be diagnosed based on appearance or behavior alone. Necropsy (animal autopsy) is the most accurate method to date scientists have. Some of the clinical signs of CWD observed at necropsy have been:
- Esophageal dilation
- Signs of excess regurgitation (damage to throat and esophagus)
- Aspiration pneumonia
- Watery and frothy rumen contents
These are also non-specific clinical signs, so further microscope is necessary for an accurate diagnosis. True CWD infected brain tissue will show:
Lesions in cells of the medulla oblongata and surrounding tissue of the brain
Astrocytosis (an abnormal increase in the number of astrocytes [supporting cells of the central nervous system] due to the destruction of nearby neurons, amyloid plaque (a hard, insoluble accumulation of proteins that clump together between neurons)
While some animals infected with CWD may die directly due to the disease, most often death is because of indirect factors. CWD- infected animals are more likely to succumb to vehicular and predator-related fatalities, be killed by hunters, or suffer secondary infections (like aspiration pneumonia).
Because of the long incubation period and slow progression, noticeable impacts on an area’s cervid population do not occur immediately. The concerns are that these impacts in population will occur years and decades after CWD’s first introduction into a new area. To date, CWD has not caused severe population declines in wild cervid populations. But some localized populations in heavily infected areas where CWD has been present for years are beginning to experience this.
Geographical Distribution
According to the Center for Disease Control (CDC), as of January 2020, CWD has been identified in 26 states (in the Midwest, Southwest, and limited areas on the East Coast), four Canadian providences, Norway, Finland, Sweden and even South Korea.

Figure 3: A map of North America displaying the spread of CWD from 2000 to 2019. The color indicates the different decades.
The origin of CWD in northern Colorado and southern Wyoming is still unknown. Exactly how the disease has spread so far over the past several decades is also unknown.
The geographical distribution of CWD may be considered as two different lineages:
- The slow dispersion among free-ranging cervids
- The more rapid dispersion within herds of captive cervids
The overall occurrence of CWD that is known in free-ranging cervids is relatively low (usually less than 10%). However, several locations where the disease is established and has been present for several years, the infection rate can jump up to more than 25%. These numbers pale in comparison to those seen by captive cervid herds; some with infections reported being as high as 79%. Identification of CWD in captive herds has sometimes preceded or overlapped with the detection in free-range herds in the same geographic area suggesting transmission occurs through the environment. Areas like Wisconsin, New York, and West Virginia have shown high concentrations of CWD in small areas suggesting the infection originated from an imported animal or some other unidentified source.
Transmission
Transmission of disease can occur in a few different ways:
- Direct transmission – the spread of a disease through contact between two or more animals
- Indirect transmission – the spread of a disease through contact with surfaces or objects that carry the infectious material (called fomites)
- Horizontal transmission – the spread of a disease through contact with excreta (saliva, urine, feces, blood)
- Vertical transmission – the spread of a disease through reproduction from mother to offspring
Important factors in determining the transmission rates of disease between animals and/or humans:
- Dose (amount of infectious material)
- Strain of the disease
- Route of infection
- The stability of the infectivity inside and outside the host
- The efficiency of its delivery to the nervous system
- Homology (similarities in shared evolutionary ancestry) between the source and recipient species
For CWD and all other TSEs, similar animal species are necessary for transmission between the host and recipient organism. Currently, there have been no cases of CWD transmitting to non-cervid or humans. Differences between species have been shown to act as a barrier to the transmission of prion diseases. Differences in the amino acid sequences between the misfolded structures of the PrPs from infected cervids and the normal functioning PrPs of non-cervids (including humans) offer the best evidence for these species’ barriers. However, over time mutations can occur and potentially overcome these species barriers (more on this in the following sections).
The transmissibility to other species is an area of research that is on-going and constantly changing. Concerning CWD, direct, indirect, and horizontal transmission are the areas of most concern; vertical transmission appears to be irrelevant. Many of the symptoms of CWD involve the release of excreta from the infected animal into the surrounding environment. This means CWD is readily spread indirectly via fomites through the environment (see Figure 4); more information on this will be presented in the next section.

Figure 4: CWD prion ecology. Shown is the potential movement of CWD prions in the environment.
CWD can remain viable for long periods in the environment and spread to other animals. The potential for cross-species transmission of CWD from wild animals to livestock (cattle, swine, sheep, etc) may increase as a result of increased shared land. The natural migration (or unintentional relocation) of wild cervids puts them in direct contact with areas where livestock roam and graze. There are also concerns about the spread of CWD by hunting and the consumption of infected cervids by wild predators and by hunters.
At this time, laboratory experiments have demonstrated strong species barriers between infected cervid cells and cells from cattle and sheep. Studies did show potential transmission could occur between cervids and field mice (voles). CWD could have the potential to pass through the species barrier to an animal that humans eat or come in contact with more readily.
The increasing spread of CWD over the past several decades and its definitive links to other TSEs, like BSE and CJD has raised concerns about its potential spread to humans. Laboratory studies assessing the susceptibility of primates to CWD have been conducted. Squirrel monkeys have been proven to be susceptible to CWD via intracerebral (within the brain) and oral routes. Though humans and the majority of primates share greater than 90% of the same DNA, they are not a reliable predictive model for human beings concerning the transmission of prion diseases.
Other scientific studies have taken a closer look at human populations that reside in heavily infected CWD areas, specifically hunters and people who regularly consume game meat. All studies completed so far conclude that there is no strong evidence linking hunting practices or the consumption of game meat to an increase in prion disease in humans. However, the possibility that CWD can cause disease in humans cannot be eliminated. The foodborne transmission of BSE to humans indicates that species barriers may not completely protect humans from animal prion diseases. The CDC recommends no one consume meat from a known CWD-infected animal.
It is currently unclear whether CWD prions pose a threat to non-cervid species or humans. Despite notable species barriers currently existing, they are not absolute. Prion diseases are dynamic and constantly adapting and the level and frequency of human and animal exposure to CWD may increase. Far more study and research are needed.
Environmental Contamination and Persistence
Environmental contamination has played a pivotal role in the spread of CWD throughout North America (Figure 4). When CWD is first introduced into a population, direct transmission accounts for the majority of new infections. Once the disease establishes itself within the area, indirect and horizontal transmission becomes the main vectors for spreading it. As previously mentioned, CWD prions are shed from infected animals through saliva, urine, feces, and blood. Once the environment is contaminated with CWD, it will remain infective. Preventing additional cases and the spread of the disease has been proven to be extremely difficult.
CWD-infected prions are remarkably stable in the environment. These prions persist for many years due to their hardy biochemical properties and ability to bind to soil (especially clay and quartz). Interestingly enough, the amount of these soil types is in high amounts in areas where CWD is prevalent. Once bound to soil particles, the prion has little mobility keeping it close to the surface thus, increasing its potential contact with grazing herbivores. Soil-bound prions are also believed to be more infectious than unbound prions. Because of this ability to persist for long periods, the physical presence of an animal within a herd is not required to spread the infection. Animals housed in pens previously occupied by CWD positive cervids have contracted the disease. Sites where cervids congregate such as mineral licks, areas for winter yarding, baiting sites, and wallows (muddy areas where deer like to roll) are all potential reservoir and transmission points.
Additionally, carcasses and gut piles left by hunters are significant contributors to indirect and horizontal transmission. Depending on the location of the carcass, the weather, and time of year, complete carcass decomposition can range from just a few days to a few months. The first way is through direct contact with susceptible cervids. In the wild, deer have been observed visiting and even scavenging decomposing cervid carcasses. The second way CWD can be spread from infected carcasses is through the soil. During decomposition, animal carcasses release nutrients into the surrounding soil, stimulating the growth and flush of subsequent biomass vegetation which attracts more herbivores to the infected area. The last way carcasses can spread CWD is indirectly through scavengers. This is done through the consumption of infected materials and subsequent spread into the surrounding environment through droppings. Carcasses provide a ready source of protein for both mammalian and avian scavengers. Studies show carcasses are routinely scavenged and visited by a broad range of mammalian and avian species. Mammalian scavengers like wolves, coyotes, raccoons, opossums, skunks, and rodents, and even more domesticated animals like dogs and cats have all been observed visiting and scavenging deer carcasses. Though avian species are not susceptible to mammalian TSEs, they can still consume TSE-infected material and spread prions or other infectious agents through the deposition of feces in the environment. On the other hand, scavengers do remove significant number of potentially infected materials thus reducing the amount of infected materials susceptible cervids may be exposed to. Regardless, deer carcasses and gut piles (unless proven to be CWD negative) should be considered a source for spreading infected prions and a contributor to increasing interspecies and potential cross-species transmission of CWD.
Evidence for Different Strains
Through research, different strains of CWD prion have been identified. They differ in the length of the incubation period, length of the disease course, lesion distribution within the brain, range of clinical signs, and its prevalence in certain species of cervids. At this point, all cervids are considered vulnerable to CWD but certain species appear to be more or less susceptible to infection than others. New strains may emerge through prion mutation and adaptation leading to new or worsening symptoms, shorter incubation periods, or the passage through cervids into new animal species and potentially humans.
Conventional and Experimental Detection
Historically, diagnosis and confirmation of CWD were dependent on postmortem sampling of brain tissue and verification via microscope of spongiform structures. Though highly valid and accurate, this method can only be applied late in the course of the disease and, most notably, is only applicable to deceased animals. Detection methods for CWD have evolved to be able to detect the disease at earlier stages and focuses more on the sampling and examination of tissues from the lymphatic system. Research continues to develop tests with higher sensitivity and that can be applied to other tissues of the body while the animal is still alive.
Management Practices
Current CWD management practices have been tailored to the two different cervid populations: farmed and free-range. Farmed cervid populations are similar to any other model of animal agricultural production. Free-range populations present a far more challenging and problematic dilemma.
- Farmed
- Individual animal identification
- Annual herd census
- Postmortem testing of all animals
- Quarantine of suspected or confirmed CWD-positive animals
- Increased biosecurity efforts by farm managers, farm employees, and veterinarians
- Free-range
- Increased sampling and detection efforts
- Head collection containers
- Free for hunters
- Placed on or near state game lands
- Testing:
- Hunter-harvested animals
- Escaped farm cervids
- Animals killed by motor vehicles
- Animals showing any clinical signs of CWD
- Head collection containers
- Hunter education
- Outreach programs, especially in at-risk areas
- Decrease feeding and baiting practices
- Population reduction (decrease direct transmission)
- Increase public hunting
- Extend hunting season
- Increase antlerless and antlered tag allocations
- Removal of antler point restrictions
- Allow nonspecific culling or sharpshooting of herds
- Increase public hunting
- Increased sampling and detection efforts
Population reduction has decreased direct transmission and proven successful in a few areas (Illinois and New York), but overall has not slowed the spread of the disease. The high levels of environmental contamination and subsequent transmission of CWD cannot be slowed only by the current management practices. There should be more practical and readily available methods to permanently remove infected prions and decontaminate the environment.
Safety Measures for Hunters and Meat Processors
General Precautions:
- Do not shoot, handle or consume any animal that acts abnormal or shows any sign of illness (see pathological signs section)
- Ensure the meat from positive-testing or suspected animals are not allowed to enter the human and animal food supply
- Take caution when handling or processing an animal (assume it is infected and treat it as such)
- Wear Latex or rubber gloves when field dressing and when breaking down or further processing the carcass
- Minimize the handling of all high-risk tissues and organs especially those located in the head and spine (Table 1)
- Normal field dressing coupled with boning out a carcass will remove most, if not all, of these body parts including the lymph nodes located in the fat and membranes around organs and joints (Figure 5)
- Remove as much fat, connective tissue, membranes and lymphatic tissue as possible
- Avoid the consumption of all high-risk tissues and organs (Table 1)
- Do not move live animals, carcasses or parts out of a disease management area (DMA)
- Carcasses and parts (especially the brain and spinal cord) should be properly disposed of while in the DMA
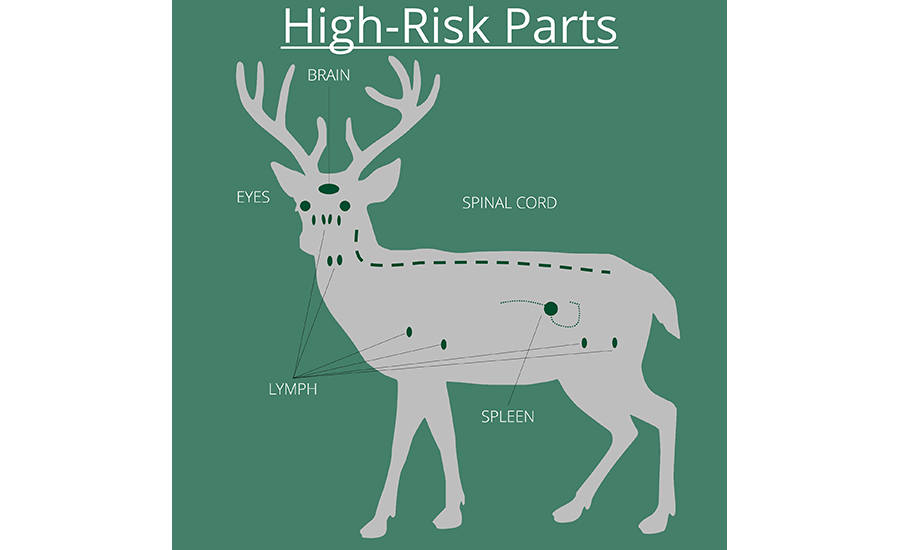
Figure 5: A diagram showing the anatomical location of CWD high-risk tissues.
Hunters (specifically):
- Decrease or stop the use of natural urine-based attractants (potential carrier of infected prions)
- Have your game tested and share the results with the processor
- Wait for the test results before having the animal(s) processed or before consuming it
- If your animal is being commercially processed, request that your animal is processed individually, without mixing meat from other animals
Processors (specifically):
- Require hunters to have all animals tested before handling and processing
- Have dedicated knives and equipment for processing game meats
- Bone out ALL the meat from the animal
- Do not saw through bone, especially the head or the spinal cord
- Thoroughly clean and sanitize (more details below) all knives and equipment in between every individual animal (unless the animal(s) tested negative for CWD)
Inactivating Contaminated Equipment and Surfaces
Hunters, meat processors, taxidermists, and others in contact with potentially infected CWD carcasses and tissues need a practical method to decontaminate and clean knives and other processing equipment. As previously discussed, prions are notoriously difficult to inactivate. Most methods that are effective are either dangerous and caustic or very expensive and not readily available (irradiation, heat, autoclaving, chemicals, enzymes).
Water alone is ineffective at removing prions; spraying or soaking does nothing to remove dried on tissues or decrease prion amount. Bleach (sodium hypochlorite [NaClO]) in high concentrations has been shown to inactive CWD and other TSE prions. A five-minute treatment with a 40% dilution of household bleach is effective at inactivating prions on stainless steel surfaces (at a 10-4 [1/10,000] and 10-2 [1/100] dilutions). For easier mixing and increased efficacy, use a 1:1 solution of household bleach (with a ≥6% concentration) and water and allow the items to soak for at least five minutes; increasing the treatment time will increase the efficacy. Prions suspended in water are much easier to inactivate. Treatments with a 10% bleach concentration or higher with a one-minute treatment or longer is effective at inactivating prions suspended in water. Bleach however has poor penetration into tissue and much lower efficacy when organic matter is present meaning it is ineffective at inactivating prions on solid tissue surfaces. Therefore, it is very important to remove all solid and visible tissues from equipment before applying a bleach disinfecting treatment.
Recommended Cleaning Procedure:
- Rinse all knives, equipment, and surfaces with cold water
- Apply a 1:1 solution of household bleach (with a ≥6% concentration) and cold water to all items and surfaces
- Soaking items in the solution is more effective than spraying on it in the surface
- Let all items and equipment set undisturbed for at least five minutes
- Increasing the treatment time will increase the efficacy
- Rinse all items and surfaces with cold water
- Proceed to clean and sanitize all items and surfaces as normal
- When finished processing, apply the bleach solution to all floors and drains
- Let floors and drains sit undisturbed for at least five minutes
- Increasing the treatment time will increase the efficacy
- Rinse everything down the drain
Note: Bleach has an expiration date and loses efficacy from exposure to light and heat (>77°F) fairly quickly if not stored properly
Disposal Measures for carcasses and parts of known or suspected positive-testing animals:
- Landfill
- Burying (at the kill site or within the DMA if applicable)
- Incineration
- Alkaline Digestion
*Always check with your area’s game commission or other wildlife management organization for the most appropriate procedures, especially if you are in or near a DMA.
Future Prospects
- Construction of a successful vaccine target and strategy
- Essential to stop the problem at the source
- Difficult to overcome the natural barrier to antibodies development (tricking anti-bodies to fight against something native to the body)
- Creation and application of an effective environmental clean-up protocol
- Crucial to slowing the transmission of the disease to other cervids and potentially onto other species including humans
- Development of a true live-animal test with greater sensitivity than current postmortem methods
- Immunoassay for tonsillar or rectal lymphoid tissues
- Create tests for blood, saliva, nasal swabs, urine or feces
- Decrease the need for physical contact with the animal through sedation or restraint
- Explore the ability to rapidly distinguish different strains of CWD
- Uncover how certain species of cervids are more susceptible to infection than others
- Identifying and selecting resistant cervid genotypes to breed
- Better understand how the disease has spread and help predict where it could go
- Be able to better detect the development of a new strain or the introduction of a strain in a new area
- Uncover how certain species of cervids are more susceptible to infection than others
Conclusion
It is not entirely clear if CWD can infect non-cervid animals or humans. At present, species barriers appear to prevent transmission from happening, but prion diseases are dynamic and constantly evolving. There is no scientific evidence that CWD will dissipate naturally over time. Evidence suggests that once the environment is contaminated, it will remain infective for an unknown period of time. Doing nothing will only result in the disease increasing in known areas and spreading to novel areas.
Action must be taken to prevent CWD from becoming an even more wide-spread problem in the future. Aggressive surveillance is necessary to prevent CWD from spreading and stopping infected carcasses from entering the human and animal food supply. Much has been learned about CWD since its discovery more than 50 years ago, but even more must be done if we hope to combat this disease. It is important to stay informed because the information is constantly being updated on CWD research. Hunters and processors should consult with their local wildlife and game agencies to identify areas where CWD has been detected and to get the most up-to-date information. Other Resources Available include the CDC, the Center for Infectious Disease Research and Policy (CIDRAP), and the USDA Animal and Plant Health Inspection Service (APHIS).
References
Evidence of a Molecular Barrier Limiting Susceptibility of Humans, Cattle and Sheep to Chronic Wasting Disease – G.J. Raymond, et. al., 2000
Chronic Wasting Disease and Potential Transmission to Humans – Ermias D. Belay et. al., 2004
Deer Carcass Decomposition and Potential Scavenger Exposure to Chronic Wasting Disease – Christopher S Jennelle et. al., 2009
Chronic Wasting Disease of Cervids: Current Knowledge and Future Perspectives – Nicholas J. Haley and Edward A. Hoover, 2015
Chronic Wasting Disease: The Basics - Walter Cook, DVM, PhD, DACVPM (Southwest Veterinary Symposium 2016)
Cross-Species Transmission of CWD Prions – Timothy D. Kurt and Christina J. Sigurdson, 2016
Chronic Wasting Disease: Emerging Prions and Their Potential Risk – Samia Hannaoui et. al., 2017
Mineral Licks as Environmental Reservoirs of Chronic Wasting Disease Prions – Ian H. Plummer et. al., 2018
Inactivation of Chronic Wasting Disease Prions using Sodium Hypochlorite – Katie Williams, et. al., 2019
Figure 1 - https://www.slideshare.net/hillcountrychapter/chronic-wasting-disease-101-by-dr-bob-dittmar-v2018
Figure 2 - https://www.theharlemvalleynews.net/?p=39989
- https://fw.ky.gov/Wildlife/Pages/Chronic-Wasting-Disease.aspx
Figure 3 - https://news.cornell.edu/stories/2019/07/expert-testifies-deadly-deer-disease-house-committee
Figure 4 – The Ecology of Prions – Mark Zabel and Almee Ortega, 2017
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!





